Setting limits on health care may be the only way to save it. What the rest of us could learn from a small American state that tried – and failed – to tackle the toughest choices on medical costs
By Ivor Shapiro
With additional research by Ellen Lupu and Leigh Doyle
The Walrus, November 2004
Five years ago, an American internist and health-care researcher named Peter Ubel wrote a book called Pricing Life: Why It’s Time for Health Care Rationing. His thesis: someone had to put the brakes on the rising cost of medical treatment, and that someone was the ordinary physician. Doctors, Ubel argued, should think about cost even as they consider their patients’ welfare, and should somehow balance these two responsibilities. The book never hit a best-seller list, and it was largely ignored by reviewers.
These days, though, its author occasionally gets invitations to speak outside the University of Michigan at Ann Arbor, where he teaches. Here is Dr. Ubel now, speaking on the wrong side of the Great Lakes, as a guest lecturer in a respectably filled auditorium of the University of Toronto. He begins his presentation with a straw poll. “How many here,” he asks, “think health care needs rationing?”
Sixty or seventy hands go up. Just one man–in his sixties, perhaps the oldest person in the room and the only one wearing a suit–votes no. Ubel smiles, then asks: “How many think physicians should ration care at the bedside?” The yesses are fewer now but they still, hugely, outnumber the handful of nos. “Freaky crowd,” Ubel says.
Certainly, it’s a self-selecting one, composed of students and teachers in the university’s department of Health Policy, Management and Evaluation. For people like this, and a slowly growing number of others mostly of the genus policy wonk, rationing is no bogeyman. Rather, it’s an unsavoury reality, a necessary response to a notion that is inching its way into popular consciousness: the “unsustainability” of health care as we know it. This idea is closely linked to another unwelcome reality: our ageing population (the proportion of Canadians aged fifty-five or over is expected to rise from 22 percent in 2001 to 32 percent by the year 2020). An older citizenry means higher costs: already, people over sixty-five, who comprise just 12.6 percent of the population, consume nearly half of all hospital costs. And our average age is going to keep climbing, thanks in part to medicine itself. Constant advances in treatments and medical technology ensure that another death-defying cure will always be around the corner. And it will always cost money.
Meanwhile, the cost of existing treatments keeps going up. Peter Ubel flashes a series of PowerPoint slides to make his case. Cost of cholesterol drugs: up 63 percent in one year. Cost of analgesics: up 16 percent. Antidepressants: up 32 percent. Proliferation of mri machines: 61 percent in two years. Of pet scanners: 88 percent. The figures are American, but as he reminds the audience, Canada, too, is one of the top spenders in the world when it comes to health care.
For every dollar in the Canadian economy, a dime is spent on health care. Last year, a total of $121.4 billion was spent by federal and provincial governments under the heading of health, an increase of 4.6 percent over the previous year, according to the Canadian Institute for Health Information (cihi). And, while governments spent $3,839 on health care for the average Canadian, the number rose to over $17,000 for people aged eighty-five and over. The Conference Board of Canada worries that the overall health bill is currently growing 25 percent faster than the economy, though if you look at the trend line since the Eighties–rather than just during the past five years, which saw an injection of government funds after several years of cutbacks–the average growth is just 2.5 percent a year.
Whatever the exact numbers, it’s a lot of money. Money that won’t be going to schools, roads, sewers, peacekeeping, or AIDS aid to Africa. Money that we’ll all be paying in taxes, rather than on clothes, computers, or camp fees for the kids.
Unless we start thinking differently about health care.
Peter Ubel says we have to start doing just that. Doctors, he says, should check the price tag before ordering drugs and tests. Take fetal ultrasounds. “My wife had two thankfully normal pregnancies,” he tells the crowd at U of T. “Of course we had ultrasounds done, even though no study has ever shown it does any good?. With insurance, it’s a subsidized baby picture. [But] if we’d had to pay for it, I’d have said, ‘Give me a dvd player.’” Similarly, a routine pap smear every three years is enough to catch almost all potential cervical cancers; an annual smear costs $600,000 for each year of life saved through all those additional tests. That, Ubel suggests, is pricing a single human life too high.
But is it? The very idea of pricing life strikes most of us as a moral road that leads straight to hell–as perhaps it should. What doctor, knowing that she might cure a dying patient, wouldn’t do everything she can? What patient, offered that cure, wouldn’t jump at the chance?
A few years ago, I started wondering if questions such as these are as self-answering as they appear. It wasn’t anything to do with money that launched me on this track. It was the dying of three fathers.
Right now my whole generation is watching its parents die, but they don’t all die as hard as three octogenarians in my family. My own father has been dying for years, depressed, incontinent, and in seemingly untreatable pain. None of his specific ailments is fatal; I guess he’s dying of “old age.” My wife’s father died with Alzheimer’s Disease; I like to remember him as a tall, kind-eyed, wide-smiling man, the sort of person about whom people use the word “dignified,” but a more recent memory is of visiting him in a locked chronic-care ward where I found him wandering the hall, clothed in bewilderment, a diaper, and an open-backed gown. A year or so later, my brother-in-law Joe’s dad had a massive stroke that crippled his limbs, erased his memory, and eventually rendered him comatose, with antibiotics, food, and air pumping into him through tubes.
By the time he died, he had, in Joe’s words, “zero quality of life.”
Zero. A low number, but still a number. It seemed to suggest that we human beings are capable of comparing life to death and, sometimes, finding death preferable. It seemed to suggest that there is a place–definable in mathematical terms–where living is worse than dying. In light of the dying I had been witnessing, this possibility no longer seemed far-fetched.
And then I started thinking something else, and I’ll admit that at this point my thoughts made me feel a bit queasy, a little like a hungry castaway catching himself eyeing a companion’s corpse. What I found myself wondering was this: might the notion of zero quality help us as we think about health-care costs? Every patient “cured” will die another day, probably not before getting older and sicker and consuming yet more money on hospital beds and drugs and medical fees. What will happen when silver-bullet cures are found for cancer and the flu? Will we then all die even later and longer and harder, of “old age,” adding to the national debt, stealing tax money from our grandchildren’s education and from the safety of our children’s roads in order to slow down–that is, lengthen–our own wasting away?
But what’s the alternative? Rationing? The word has never in history rung a pleasing note; applied to health care, it’s positively discordant. Today, the R-word shrieks like a scorned soprano whenever governments trim health costs. Last spring, when Ontario’s Liberals buried within their budget speech two sentences cutting universal coverage for routine eye exams and what remained of physiotherapy and chiropractic benefits, the opposition, of left and right stripes, united to attack the cuts in the legislature every day for a week. Voters want more medical attention, not less: no one wants to think of health science the way we think of road repairs or even schools. Could the idea of placing limits on medical care ever, ever, get tuneful enough to hit the political agenda?
Well, there was one time, one place, that it did. The place was the State of Oregon, and its unique story, a story of unspeakable questions being asked and answered in the most public way, starts with the cruel death of a little boy.
His name was Coby Howard. He was seven, he had leukemia, he had a cute, telegenic smile, he lived in the town of Rockwood, and he was poor enough to get government health coverage within the Medicaid system.
Except, Oregon had, in June of the year of Coby’s death, joined a handful of other states–and many private insurance schemes–in withdrawing funding for most high-end transplant services. That included the bone-marrow transplant that might, just possibly, have saved the boy’s life. Heart-wrenching TV appearances, citizens’ petitions, and a massive fundraising effort followed his diagnosis, all to no avail. He died in June, 1987. And then, something new happened.
In politics the world over, there is a template for matters of this kind, and it runs like this: 1. Government makes a controversial decision. 2. Tragedy results. 3. Public is outraged. 4. Government backs down. So, shortly post-Coby, the Oregon legislature’s emergency board assembled to debate a motion to restore $700,000 (U.S.) for transplants–enough for eight or nine Medicaid patients. The charged debate took place under the gaze of the U.S. national press, which reported that while the politicians mulled, transplant patients were begging for their lives or crossing the Columbia River for surgery in Washington. Coby’s aunt Susan appeared before the emergency board and said (according to The Washington Post), “I asked him to smile for the cameras, when not thirty minutes before he had been vomiting?. I had to turn Coby Howard into a product so the public would buy him his life.”
And that’s where Oregon started down its new trail. The legislators, by nine votes to seven, said no to the transplant funds. The leading “no” voice came from Dr. John Kitzhaber, the president of the state’s Senate, whose day job was as an emergency-room physician. The $700,000 might perhaps save a few lives, Kitzhaber said, but would be better spent elsewhere. For instance, on primary health care for the more than fifty thousand kids in Oregon who had no health insurance at all, kids whose parents waited until they got really sick and then arrived–sometimes too late–in emergency rooms such as Kitzhaber’s.
So, the doctor said, let’s do something different here in Oregon. Let’s provide less health care, for more people. Let’s ration–yes, ration–health coverage. And when the post-Coby debate ended, he started putting flesh on the bones of his big idea. Roving the state in blue jeans and cowboy boots, he assembled a small group of health-policy advocates and lobbyists to frame a plan based on a simple notion: Oregon should move toward basic health coverage, not just for the poorest of the poor–a family of four earning $7,260 (U.S.) a year or less, according to the state’s Medicaid guidelines–but for every resident of the state.
Universal health care. It was a radical notion in Kitzhaber’s country, but it could be achieved, Kitzhaber said, without raising taxes. How? By reallocating health-care resources. Kitzhaber’s plan would first limit Medicaid coverage to “basic” services, including those that prevent illness and those that fight it most effectively. The dollars saved would be used to offer the same set of basic services to everyone living below the federal poverty level, which was then $12,100 a year.
Meanwhile, a law would be passed mandating every employer in the state to provide health insurance covering, at minimum, the same package of basic services. And, to keep premiums affordable, the state would help take care of people with especially expensive medical needs. Since self-employed middle-class people and the independently wealthy could be expected to buy their own basic coverage, the dream of health care for all seemed suddenly within reach.
It was a highly original idea, so, of course, thousands hated it. Right away, the idea of covering only “basic” services under Medicaid sparked fury across the United States. Oregon was rationing health for the poor! AIDS treatments would go first! Care would be denied to those who needed it most! Senator Al Gore was reported as saying the plan offended “fundamental fairness and decency.” The Catholic Health Association, the Epilepsy Foundation of America, the Gray Panthers, and The Children’s Defense Fund (board member: Hillary Clinton) voiced outrage.
But within Oregon, Kitzhaber quietly won–apparently by cold logic–the support of his fellow Democrats, many Republicans, doctors, hospitals, big business, small employers, and health insurers. By May, 1989, he and his followers had pushed through the Oregon Basic Health Care Act. The law required Oregon to create a Health Services Commission that would rank all (!) known health treatments in priority order. On this List, the Legislature could then draw the line between basic–that is, affordable–services, and the rest.
Above the rationing line, there would be health care for everyone. Below the line, the state would say no, and the law of the Wild West would rule: it would be everyone for themselves.
—
I don’t remember exactly when I first heard about Oregon’s experiment: an ethicist friend mentioned it perhaps a decade ago, near the beginning of the adventure. Only much more recently did I cotton on to the broader story about rationing–that its existence is by no means confined to a 96,000-square-mile slab of Pacific Northwest.
The truth is, health care is rationed daily, and everywhere. It’s simply the only way there is to match the supply of medical miracles to the demands of sick citizens. The rationing criteria vary, as do the logistics, but the principle is the same: we can’t pay for all people to get everything, so we find ways to say no to some people, or some things. The biggest question raised by Oregon, and being explored by some policy wonks, is whether the process should be strategic and explicit, or ad hoc and hidden from the public eye.
Almost everywhere in the world, it’s the latter. The United States, for example, rations by income level, age, and disability. If you’re comfortably employed or endowed, you get private health insurance; if you’re poor enough, old enough, or disabled enough, you may get federally subsidized Medicaid and/or its senior-citizen partner, Medicare. Otherwise, you get the emergency room or, if you’re lucky, a crowded, resource-starved, community health centre.
In Canada, on the other hand, we ration in two distinct ways. First, by the profession of the provider: nationally, we cover doctors and hospital services, leaving most of the country’s nurse practitioners, dentists, physiotherapists, chiropodists, and midwives to bill privately. And second, we ration by means of waiting lists. Need an MRI or radiation therapy or a specialist appointment? Take a number.
This system has both strengths and weaknesses.Prime Minister Paul Martin campaigned for re-election in June by playing (with arguable success) on the widespread belief that waiting lists are inherently evil, and his government continued to trumpet that cause during health-care negotiations with the provinces into the fall. But a well-managed waiting list need do no harm. Dr. Michael Rachlis, Canada’s leading health-policy guru, writes in his new book, Prescription for Excellence: How Innovation Is Saving Canada’s Health Care System, that transplant and cardiac-care waiting lists match priority to urgency with life-saving results. Many other wait times, he says, could be cut, without additional cost, by fixing inefficiencies in the way queues are managed.
As for selecting among providers’ professions, the case for drawing a line somewhere seems obvious. If chiropractors and psychologists got billing numbers, why not registered massage practitioners and hypnotherapists? Rachlis, for one, argues that the line is artificial and arbitrary. Science often favours non-MDs, he says; routine optometry has been proven to prevent vision problems, and chiropractors do best at managing low-back pain.
Logic suggests, then, that a less arbitrary approach to rationing might not only cost less, but also improve the quality of patients’ care. But logic rarely wins votes, and in Canada, reason brushes up against an amorphous but powerful force: our national identity. Canadians believe in their health-care system. It’s one of the things that distinguish us from our neighbours to the south, and from much of the world. To have been caught tinkering with the Canada Health Act would have spelled death to any party in the federal election last spring, and so no one proposed doing so (beyond, perhaps, suggesting adjustments to the role played by for-profit operations). Rather than facing up bravely to the reality of rationing, we may prefer the lie that our Canada includes universal, comprehensive health care.
It is–no question–a lie. Health care in Canada is a compromise arrangement between political reality and the vision of Justice Emmett Hall’s Royal Commission report in 1964. Hall had proposed comprehensive coverage for medical services, drugs, and home care, and for dental and optical services for kids. The Trudeau government sawed it off at medical services, and some (not a lot) of the rest gets covered (sort of) by some provinces. The 1984 Canada Health Act made it official: to get federal funding, provinces need only cover physicians’ and hospitals’ services–and only those deemed “medically necessary.”
“But what the heck does that mean?” asks Colleen Flood, the chair of health law research at the University of Toronto. It’s Flood’s job, right now, to untangle that knot, because she and two colleagues have received grants from the federal and Ontario governments to lead a three-year research project called “Defining the Medicare Basket.” The idea is to investigate what health care services should be publicly funded, as well as consider who decides about that funding, and how.
Flood’s project is just one sign of a quiet momentum that is building toward restocking what health professionals call the “basket” in a more strategic, less accidental, way. In the wake of the reports of Royal Commissioner Roy Romanow and Senator Michael Kirby last year, Ottawa and the provinces agreed to move toward national coverage for home care and drugs. Whatever deal is finally struck, it’s either going to cost serious money or force cuts to existing services. Over the years, provinces have, with relatively little fuss, denied funding to items such as cosmetic surgery and in-vitro fertilization. But what’s next? Hip replacements? Knee surgery?
Flood’s point is that if we’re going to take up costly new initiatives such as home care, and keep pace with new medical innovations, some things have got to go. “Like what?” I asked. Like annual general checkups, Flood answered. “There’s no evidence that there’s any health benefit at all from an annual general checkup,” she said. But we fund that, while we don’t, across the board, fund childhood vaccinations. “Some provinces fund chiropractic pediatric neck manipulations, which some people think is actually dangerous. But we don’t have universal access to insulin.” She paused. “So we have a pretty weird system.”
Weird, in part, because the system is hidden and mysterious to practically everyone involved. The federal government stays out of the business of defining “medical necessity,” leaving the provinces to determine (by a process few understand) the list of services for which physicians can bill. Within that framework, it’s left up to the nation’s doctors to decide what’s “necessary” for individual patients.
Is this a bad thing? You decide. A landmark study known as the Dartmouth Atlas found stunning variations in treatments ordered by U.S. physicians. Doctors in some regions were six times more likely to prescribe surgery for chronic back pain than elsewhere. Differences were almost as large for lumpectomy and mastectomy. Overall, spending on traditional, fee-for-service Medicare in Miami was twice Minneapolis’s, after adjusting for age, race, and sex. Variations appeared to have nothing to do with the incidence of illness or with patients’ socio-economic status.
So, what’s medically necessary? If doctors disagree so much, what hope is there for prioritizing health care? The answer, again, may lie in Oregon.
—
The State House in Salem is topped by a rippled marble fez that’s nothing like any other legislature’s dome–an architectural signal, perhaps, that Oregon likes being different. “Oregon is not really in the United States,” Peter Ubel told me when I asked him about the state’s nervy health-rationing move, which is a funny thing, when you consider that the Oregon Trail was, at one time, a potent symbol of the American spirit: for years, the image of tens of thousands of pioneers setting out in their wagons from Independence, Missouri, headed for the great Northwest, defined America’s can-do individualism, its notion of a manifest destiny.
The Oregon of today is much changed, of course, but it does retain its frontier identity: the state was first in the U.S. to legislate bottle refunds for beer and pop, first to see same-sex couples married legally, among the first to allow medical use of marijuana, and first (and only) to allow physician-assisted suicide. Toward the end of a day’s drive down to Salem, from Vancouver, I explored the state’s beaches and coastal hills; on a previous visit, in winter, I had breathed the mossy air of the Columbia Gorge’s vertical forests. But the thing I had really come here to see was on the fifth floor of the Human Services Building, just east of the great fez: a filing cabinet that would offer me a glimpse of the way the Health Services Commission set out to prioritize medical treatments.
This record is less dreary than you might expect. Filed the way they came off the old continuous-feed printers, each page inverted to the next, the minutes at times evoke the drama of ordinary people (five physicians, a nurse, a social worker, and four mere citizens) tackling something unprecedented. I asked Commissioner Ellen Lowe, a grandmotherly, Lutheran, social-services activist who drinks her martinis dry, to tell me what that was like. “It was a time of great optimism,” she said. “We had a sense that we were building a roadmap rather than following [one]. I looked at it as an opportunity to be a pioneer in health care.”
The commission started work in September 1989, beginning a year-long series of public meetings to which hundreds of citizens flocked in order to give testimony, their concerns and suggestions covering AIDS and prenatal care, dentures and kids’ cavities, naturopathy and transplants. While all that was going on, the commissioners ordered up what must surely be one of the more quirky public-opinion polls in history. Students from Oregon State University took to phone banks to ask one thousand citizens how they felt about a long list of conditions–seizures, burns, reliance on a wheelchair, problems with hearing or sex, itchy rashes. “If you feel the situation describes good health,” the pollsters said, “give it a score of hundred. If you feel it is as bad as death, give it a score of zero. If the situation is about halfway?,” and so on. The results provided made-in-Oregon “quality of well being” weights (called qwb) for symptoms and side-effects.
Meanwhile, a subcommittee was taking testimony from specialists in every medical discipline, teasing out a list of symptoms for each known medical condition, side-effects of each treatment, the probability of a treatment’s delaying death, and the length of that delay. Finally, the staff collected rudimentary cost-estimates. The cost of an appendectomy, for instance, would need to include the bills from the surgeon, the anaesthetist and the hospital, plus drugs, and outpatient care, and so on.
Fitting all this information into a common template for all conditions and treatments was hit-and-miss, but eventually, the commission’s computer had the data it needed. The machine took a cost-effectiveness formula that looked like this —
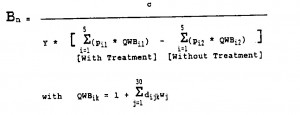
— and crunched its diet of numbers for cost, death-delay, and quality of well-being, sorting the results from most to least bang for buck. Then it dumped out its list.
“The media came to the [commission’s next] meeting,” recalls Darren Coffman, then a staffer to the body and now its director, “and out came this funny-looking ‘sort.’ The commissioners took one look at that and knew that there was quite a lot more work to be done.”
No kidding. In the fifth-floor filing cabinet, the folder containing this May 1990 “sort” is not labelled a List but a “List”– in carefully penned quotation marks. Among staff, it’s known as “The Data Dump.”
The Sort/List/Dump ran from antibiotics for bacterial meningitis, at the very top, to surgery for vulval varices, at the bottom, with temporal artery bypass surgery and treatment for traumatic head injury unfundably low down. Most famously, as Dr. David Hadorn reported in the Journal of the American Medical Association a year later, “Surgical treatment for ectopic pregnancy and for appendicitis are rated just below, or as less important than, dental caps for ‘pulp or near pulp exposure’ and splints for temperomandibular joint disorder, respectively.”
That last shocker had enough impact on JAMA’s readers that it was quoted to me, almost verbatim, by a Canadian pediatrician friend when I mentioned Oregon to him recently. This was thirteen years after the Dump, which never came close to influencing actual practice, had been stuffed forever into the filing cabinet.
Barely pausing to absorb the media’s response (which was more mixed than the medical community’s), the commissioners regrouped to find a different way to prioritize. The Dump’s method was itself dumped, closely followed by all the dollar numbers, since any cost-driven formula would suck cheaper treatment toward the top of the List and push most hospitalizations down the drain. “We just went back to work,” says Ellen Lowe, “and instead of using our computers, we used our common sense.”
That meant a more subjective process of grouping treatments with similar outcomes, ranking the groups, and then fine-tuning the List by what Coffman calls “hand-adjustment.” By winter’s end, the full commission had achieved a consensus placing top priority on life-saving treatments that promised full recovery (such as appendectomies), followed by maternity care. Then came treatments for acute fatal conditions that didn’t offer full recovery and preventive care for children. Near the bottom–ripe for the budgetary scalpel–were infertility services and treatments that promised “minimal or no improvement in quality of life.”
The new improved List, released in February 1991, ran from medical therapy for pneumonia, Line 1, to life support for anencephaly, Line 709. Later that year, the legislature made its funding call. Line 587, therapy for esophagitis, was in; Line 588, treatment for intervertebral disc disorders, was out, along with liver transplants for cancer (Line 610), counselling for obesity (Line 634), and therapy for food allergies (Line 652).
The irony of all this work is that the new List (labelled “The Big One” in the Salem filing cabinet) was quickly and quietly accepted by Oregon’s doctors and citizens. Unlike the Data Dump, it made no headlines in medical journals or elsewhere. It merely made sense.
There was just one problem. To scale back Medicaid benefits, Oregon needed federal permission. So the List went to Washington, where the minions of George Bush the First and then of Bill Clinton spent two years picking it over and demanding changes. After two rounds of amendments, the administration gave the List a reluctant nod. But it also said it would not authorize any future substantial change to the funding line. The whole idea of rationing services to match available funds was now on life-support, with the President manning the switch.
As well, the feds–for reasons too complicated to go into here–effectively vetoed Oregon’s employer mandate law. This refusal, which went almost entirely unremarked upon outside Oregon, was a crucial blow to Kitzhaber’s vision: it passed a sentence of prenatal death on universal coverage.
Nevertheless, what was left of the Oregon Health Plan was born on February 1, 1994, and despite its deformities, the state’s citizens were smitten enough to choose its father, John Kitzhaber, as their governor that same year. Times were good, Line 587 remained affordable, and about a million people received benefits under the Plan within the next decade. In 1998, the year Kitzhaber was re-elected, an editorial in The Economist described the OHP as “Oregon’s most impressive policy experiment of recent times. It works; it is popular; and the rest of the country should learn from it.”
—
A handful of states, including Utah and Idaho, have followed Oregon down the path of defining “basic” medical packages, as have national projects in New Zealand and the Netherlands. None has yet achieved its goals, and no consensus has emerged as to what “basic” necessity means or how it should be catalogued. True, Oregon figured out a way to prioritize care, and the results won approval within the state, but when it came time to sell its List to the nation, it came hard up against the most “basic” of questions–one that defies answering within the political realm. The question amounts to this: how do you measure what a person’s health–or life–is worth?
For that was the rock against which Oregon’s plan fell in Washington. Certainly, the U.S. government had some crass political reasons to kibosh the plan, but when it sought a reason to say no, its chief official reservation was hard to counter. Wrapping themselves in the flag of the Americans with Disabilites Act, the feds demurred to the value Oregon had placed on “quality of life” in building its List. Remember the students’ phone survey asking for a zero-to-hundred score for dependence on a wheelchair or problems with hearing, or the ranking of treatments that promised “full recovery” above those that didn’t? It all inescapably smacks of according less value to a life with disability.
And that’s not the only problem with the entire idea of prioritizing. Against cost-effectiveness there stands an unwritten but immutable moral principle that has been called the Rule of Rescue. (It was cited against the Oregon scheme in that influential 1991 JAMA paper.) The Rule says something like this: if, on your way to a meeting, you see someone bleeding on the sidewalk, you should stop to help. Even if your meeting is about preventing the Third World War, you should stop to help. Likewise, if your doctor can prevent your child’s death, she should do it — even if the money spent could save ten other lives.
With the Rule imprinted on all of our souls, neither doctors nor their patients want to think about health in utilitarian terms–a natural aversion that gets bolstered by something more modern and less ethical, which is the twenty-first-century Westerner’s sense of entitlement to more and better health care, along with all the other comforts of life. We’ve come to think of illness, and especially death, as an affront to human dignity: after all, the right–the right!–to life and liberty is enshrined in the constitutions of civilized states.
There was a time when people thought rather differently about illness and dying. In the Middle Ages, as Michael Rachlis writes, “death was so common”–I think he means something like undelayable–“that it was a visible part of communal life. People died at home. As death approached, they got their affairs in order–forgave long-standing conflicts, wrapped up legal and financial issues, and spoke final words to loved ones.” Now, too many people die like my father and those other fathers, or, maybe worse, are resuscitated with rib-cracking zeal and hooked up to machines to live longer deaths.
As things stand now, the thorny task of reevaluating medical necessity could require a prior consensus on some way not only to “price life” but to quantify “quality of life,” in the sense to which Joe, my brother-in-law, pointed. How close to “zero” do the lives of our fathers, our loved ones, ourselves, need to get before we feel at ease saying, “No: this life is worse than death”?
More than a decade ago, health economists, at least, reached such a consensus: quality of life could be measured numerically, they agreed–and measured against death. Someone even gave the proposed unit of measurement a name, and it stuck: the quality-adjusted life year, or QALY for short. Today, you can find at least 2,273 references to qaly-measurements in reputable medical journals (241 of them in the past year).
To calculate the quality-adjusted value of the past year of your own life, you would give your state of health and physical ability in that year a score between zero (think Six Feet Under) and one (Baywatch). That fraction is how much of a QALY you survived in the period under review. Given quality-adjustments of that kind for an ever-wider range of health states, researchers now feel able to measure the effectiveness of any treatment for any condition, factoring in any set of alternatives (death, disability, or discomfort) or side-effects.
And then, they can factor in the treatment’s bill, thus producing cost-effectiveness data.
Dialysis for end-stage renal disease costs $53,000 (U.S.) per QALY.
For type two diabetes, lifestyle counselling costs $51,600 per QALY gained, but prescribing the drug metformin costs $99,200.
Fitting a hearing aid comes at the dime-store price of $17,072 per QALY.
And what’s a good price for a quality-adjusted life? To judge by journal citations worldwide, the medical-research marketplace has settled on benchmarks proposed in a 1991 Canadian Medical Association Journal article lead-authored by Dr. Andreas Laupacis, who now heads the prestigious Institute for Clinical Evaluative Sciences in Toronto. To help provide “a framework with which to interpret the economic evaluations,” Laupacis proposed that where a new treatment promises to be both more effective and more expensive than existing options, it should get good marks if it costs less than $20,000–Canadian–for each QALY gained, lower marks if more, and a “D” grade if the sticker is more than $100,000.
—
Outside the world of wonks, the problem of measuring one treatment–or life–against another seems rather less settled. But maybe in the end it comes down to quantifying the Q in QALY: how much difference can disease make? how much must enjoyment decline before the death-life needle hits zero? who decides, and how?
To find answers to those questions, I took another, less scenic car trip–to steel-smoked Hamilton, Ontario, to meet Dr. Gordon Guyatt, one of the world’s leading researchers on health-related quality of life, and to sit in the subject’s chair for something called the Standard Gamble Test.
Guyatt’s research assistant, Peggy Austin, who administered the test, described a series of symptoms, at varying levels of severity, for an illness called Gastro-Esophageal Reflux Disease (a.k.a. GERD, which is more commonly known as heartburn). Assisted by a tattered cardboard visual aid she called the Chance Board (which I won’t try to describe here except to say it included a variety of shifting percentage numbers and the eye-catching phrase “IMMEDIATE DEATH”), Austin asked me, again and again in a studiously neutral voice, to choose between simply living with those symptoms and getting treatment for them. The catch was that each time she asked, the treatment in question came at a certain risk–10 percent, 20 percent, 30–of immediate death.
Guyatt politely declined comment on my responses, though he did raise his eyebrows over my choice, when confronted by the severest form of GERD (burning stomach pain by day, sleeplessness by night?), to be treated, even at a 40-percent risk of death. Most subjects, he murmured, would be more likely to choose so risky a treatment when facing the symptoms of a severe stroke.
He also said that he’s not especially fond of the Standard Gamble method of quantifying patients’ experience with diseases and side-effects. The Gamble has “gold standard” status for defining the q in QALYs, but he, personally, prefers to combine it with other, more reliable tests known by the equally folksy names of The Time Tradeoff and The Feeling Thermometer.
Guyatt works in McMaster’s renowned clinical epidemiology research department, and publishes twenty to thirty papers a year on subjects such as “Appropriateness of domiciliary oxygen delivery,” and “Summary of meta-analyses of therapies for postmenopausal osteoporosis and the relationship between bone density and fractures.” That kind of thing. He told me not to think of him as a health-policy academic type. “I’m a clinical-trial, quality-of-life, evidence-based evangelist type,” he said.
The metaphor was apt, for evidence-based medicine is rapidly becoming gospel for modern clinical practice. The idea is to give doctors at-their-fingertips data on how treatments actually work (as opposed, for example, to the promotional data that comes with new drugs). To help doctors know which colour pill actually makes patients feel better, and for a longer time, than the others.
Guyatt and others use the evidence collected to develop standard-of-care protocols for a growing number of medical conditions. These best-practice protocols allow doctors to feel more confident that they are doing good for most patients, rather than ordering every test, trying every procedure, for fear of missing the one that might work, and maybe getting dinged for malpractice when two other doctors take the stand to say what they would have done.
These protocols–not prioritization, not redefining the funding basket, not any kind of overt rationing– are the way to make medicine more efficient, says health economist Dr. Robert Evans of the University of British Columbia. “What’s chewing up the money in our system,” he says, “is not the rare and expensive procedures, but the not-terribly-expensive procedures, endlessly repeated, on people who probably don’t need it.” Meaning too-frequent diagnostic tests such as ultrasounds and mris, and expensive drugs that are prescribed when a cheap one will do.
One problem with selling that idea to MDs is, of course, that doctors don’t order tests for fun or for kick-backs. They do it because now and then the “unnecessary” test will save a life, the pricier drug avoid a low-risk side-effect. Unlike Peter Ubel, the prophet of bedside rationing, most physicians presume–as do their patients–that their job is to focus single-mindedly on the patient before them.
Gordon Guyatt agrees–despite the appeal of his Q numbers for economists. He says he’s not interested in rationing. His passion is to understand more about how treatments make patients feel. Recently he has been developing disease-specific measures to determine, for instance, how short of breath a treatment leaves patients, how tired it makes them feel. The idea, he says, is to enable doctors and patients to discuss a treatment’s quality-of-life effects and side-effects.
“Clinicians operate to a huge extent by heuristics,” Guyatt says. “We’re not good at those sorts of conversations. To a large extent, it’s, ‘You’re short of breath? I recommend respiratory rehabilitation for you. You have breathing problems: take this combined puffer that has all the airway-opening drugs in it.’”
Instead, he says, he wants to help doctors to help patients make more informed choices.
—
Choices. It was only toward the end of six months of research on quality of life that it dawned on me how it might all boil down to that one word. It’s possible to see quality of life as roughly correlated to quantity of choices. My father’s life, for instance, is distinguished by a relative lack of options: he can no longer choose when to go to the bathroom. His cognitive losses and depression make everyday decisions excruciating. As for managing his pain, the doctors say he’s out of options there, too. Subtract enough choices, and he’s heading, steadily, for “zero quality of life.”
Unless luck–or he himself–should intervene by ending it all. How he would handle such a prospect, I have no idea: the choice has never been offered to him. It certainly wasn’t in 1998, when he was diagnosed with rectal cancer and rushed into surgery. They “got it all.” They “saved his life.” Meaning, his dying was made longer. He got six years, and counting–but how many QALYs? His doctor said, “Max, you’ve got to get to the hospital,” and no one–certainly not we, his family–thought of saying, “Dad, you have a choice. You could fight this cancer, or you could accept it.” Such a choice is against human nature.
Or is it? In his third year as governor, John Kitzhaber signed into law the Death with Dignity Act, the only one of its kind outside the Netherlands and Belgium. Under rigorously defined conditions, it allowed physicians to write lethal prescriptions for patients diagnosed with a fatal disease.
Kitzhaber saw the law as part of a necessary change in the way people think of health and sickness. Society needs “a change in the mindset that death is an option,” he told me when we met last spring. Then he quoted a former governor of his neighbouring state of Colorado, Dick Lamm: “He has this speech where he talks about [people promising] ‘We’re going to defeat AIDS and we’re going to cure all deadly diseases.’ Lamm pauses and then says, ‘What are we going to die of? Rust?’”
Dr. Nancy Crumpacker, an oncologist in Portland, saw the new law as a call to open a new kind of practice–providing counsel to patients examining the exit door and to their doctors across the state. She says that after twenty-three years of watching people die painfully, it was natural for her to try to help ease or, as she puts it, “hasten” deaths. She never considered that she was trained to fight death, she says. “I was trained to relieve suffering.”
And, yes, the cost of legal suicide assistance was immediately covered on the List, under the heading of comfort care, Line 268.
But the most striking thing about the law is how seldom it has been used. In 2003, physicians wrote sixty-seven prescriptions under the law–nine more than the previous year. In the six years since legalization, just 171 patients took the prescribed drugs, out of 53,544 Oregonians who, according to the Department of Human Services, “died from the same underlying diseases.” And Crumpacker says that of those for whom she has written the prescriptions, many haven’t gone on to fill them. This does not surprise her. “Having a written prescription,” she says, “put the decision-making process in the patient’s hands, not in mine.”
In other words, the patients didn’t necessarily want to die. They wanted to take control. They wanted more choice.
—
As for Oregon’s dreams of universal coverage, well, that has all come to naught. When the state’s economy and revenues dipped at the turn of the millennium, Kitzhaber and his successor manoeuvered to keep the Oregon Health Plan alive despite Washington’s refusal to let the rationing line be raised. Finally, in a plebiscite on the eve of the OHP’s tenth birthday, in February of this year, voters rejected a vital tax increase. Benefits for the “working poor” are being phased out. Though some extended coverage remains on the books for now, it seems clear it seems clear that soon, state-sponsored health services will, once again, be offered only to the poorest of the poor, and to everyone who shows up in emergency rooms.
Thus is ending, by inches, the world’s first experiment with strategic rationing, but its failure has not come for the reasons that critics predicted. Prioritizing treatments proved both feasible and clinically acceptable, and (as everyone seems to agree) health care for the poor actually improved under the new system. The little state was simply thwarted by the limits on what one jurisdiction, acting alone, could achieve in a federal system.
Lacking the kind of leadership that can lead nations into tough choices, the rest of the world is, nevertheless, tottering toward a less adversarial co-existence with illness and death. Hospital ethicists work with doctors and families to make more overt end-of-life choices. Doctors talk privately about the need to shift focus toward quality of life. “Living wills,” or advance directives forbidding heroic measures against death, are written more frequently; palliative care has found a place as a respectable discipline.
Will these glacial shifts uncover more willingness to say no to health care? Maybe–especially as the cost of dying continues to rise. The Institute of Actuaries told the Romanow Commission that “between 30 and 50 percent” of patient costs are incurred in the last six months of life. Dr. Glen Roberts, director of health programs for the Conference Board of Canada, told me carefully that while the question of how far to go in extending lives has until now been handled privately between patients and doctors, “broader discussions” might be needed “ten years from now?. When we reach the point in time when the seniors are starting to hit our health system in a big way, and we’re using up almost 50 percent of provincial budgets, then these discussions are going to have to occur to ensure our sustainability.”
Roberts also said this: “There’s going to come a point in time when we have to do more than tinker. And when we’re talking about doing things other than tinkering, I think we have to talk about, you know, how do we let people, you know, live their lives the way they want to live, but also die the way they wanted to live?”
For now, not even Peter Ubel sees the deathbed as a place for rationing. “The hardest time to think about money is when you’re faced with a desperately ill patient who is asking for a chance at life,” he told me. “In that situation, it’s better to talk about the benefits and burdens of a treatment.”
Ubel allowed that it’s a pity so much time and effort goes to “adding years on at the end of life, rather than in the middle of life, when those years would be so much more fun to live.” But he just smiled when I mentioned the high spending estimates for the end of life. “You only know you’ve ‘wasted’ the money on the day after the person dies,” he said. “Tell me when the last six months of life begin, and we’ll stop spending the dollars right there.”
